Angela Gritti from the San Raffaele Telethon Institute of Milan talks about the efforts of applying gene therapy to one of the most difficult body organs to access.
Gene therapy is nowadays a therapeutic reality for various genetic disorders, also thanks to the important contribution of Fondazione Telethon. The progress in genetic engineering and the knowledge of the mechanisms at the base of diseases enabled the transformation of some viruses into vehicles of therapeutic DNA, which provide functioning versions of genes that are defective and therefore cause the diseases. Nevertheless, not all tissues – and hence not all disorders – are equally suitable for a therapeutic approach based on gene therapy: one of the biggest challenges in the field is reaching the brain, an organ which is wrapped by a naturally occurring membrane acting as barrier and is therefore poorly accessible.
At the San Raffaele Telethon Institute for gene therapy (SR-Tiget) in Milano, Angela Gritti has long been studying how to apply gene therapy to disorders of the nervous system that manifest in the first few years of life and for which at present there is no available cure, despite the efforts. «These disorders are mainly due to the accumulation of metabolism byproducts, which are not cleared and become toxic for the nervous cells. Frequently, there is an enzymatic defect at the root of the disease: depending on the missing protein, a specific toxic substance accumulates, damaging the brain. This is the cause of leukodystrophies and gangliosidosis: each disorder has its own peculiarity, but the shared features are dramatic. After an onset which can occur in the first few years of life, there is a progressive loss of the motor and cognitive functions, up to the premature death of the patient».
A brilliant success story of a gene therapy approach for a disorder belonging to this category comes from research developed at SR-Tiget: it is the case of Libmeldy, developed for the treatment of metachromatic leukodystrophy, which was approved as medicinal product in the European Union at the end of 2020. Libmeldy is an ex vivo gene therapy, in which patient cells are engineered outside of the body and reinfused after their correction with the viral vector. The vector is of lentiviral origin (as it derives from the HIV virus) and it is able to integrate into the host DNA, enabling a stable and long-term correction. A less intuitive but crucial aspect is that the cells which are corrected with the therapy are not the cells directly affected by the disease (namely the neurons), but the blood stem cells, which reside in the bone marrow and generate all blood cells. Indeed, some of the ‘daughters’ of these stem cells are recruited to the brain due to the inflammation caused by the accumulation of toxic substances: thanks to their ability to produce higher-than-normal amount of enzyme and to secrete it, they are able to detoxify the brain and to preserve it from degeneration, provided that the intervention is performed in the pre-symptomatic phase, when the organ damage is not irreversible yet.
Unfortunately this approach, which is giving promising results also for another genetic lysosomal storage disorder (Hurler syndrome or mucopolysaccaridosis type 1H), does not work for all these diseases. Angela Gritti indeed explains that ‘a lot depends on the structure, dimension and way of functioning of the disease-causing gene and the protein that it encodes. For example, in the case of gangliosidosis, which feature the accumulation in the brain of a specific type of fat called sphingolipid, this approach does not work and at present there is no effective and safe way to provide the brain with the missing enzyme in a sufficient amount and with the appropriate timing. Indeed, the most severe forms of this disease have a very rapid course and hematopoietic stem cell transplantation is not able to restore the production of the protein on time. For these reasons, for many years we have been studying a combined strategy that, besides the transplant of stem cells, envisions delivering the enzyme directly into the brain, this time through an in vivo gene therapy approach.
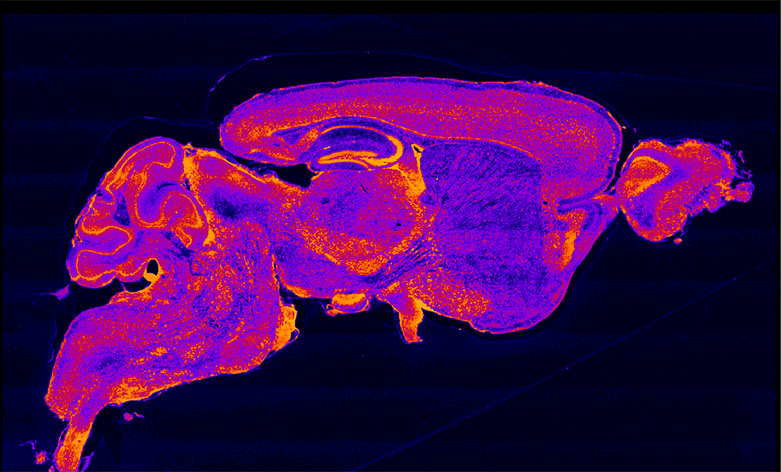
In an article just published on Molecular Therapy - Methods & Clinical Development, Gritti and her team have shown that in the animal model of Sandhoff disease (a type of gangliosidosis) the combined strategy confers a clear advantage compared to the single treatments by delivering the missing enzyme rapidly and steadily both in the central and peripheral nervous system. «When treated with this approach, the mice that mirror the symptoms of the human pathology live longer and better, show both a higher enzymatic activity and a reduction of toxic metabolites in the brain - Gritti comments. The in vivo gene therapy provides an almost immediate availability of enzyme and this enables the blood stem cells to get to the brain, engraft and start functioning, exerting also an anti-inflammatory action: for a disease with such a rapid course like this one, this is a crucial aspect. Moreover, we have identified the threshold of enzymatic activity (measured in the cerebrospinal fluid) needed in order to impact significantly on the disease, which needs to be at least 20-25% of the physiological one».
This study represents not only a critical contribution to the future development of combined therapies for the treatment of gangliosidosis but also contributes to the interpretations of the results of experimental therapies that are currently being tested. Indeed, not long ago the preliminary results of an in vivo gene therapy clinical trial for Tay-Sachs were published on Nature Medicine. Tay-Sachs is another form of gangliosidosis with a clinical course similar to the one of Sandhoff disease and it is due to the deficit of the esosaminidase enzyme: the difference between the two disorders is the portion of the enzyme involved, respectively the alpha or beta subunit. The approach used for Tay-Sachs is an in vivo gene therapy based on different AAV vectors that, differently from lentiviral vectors, do not integrate into the DNA and that were injected into a specific area of the brain and into the cerebrospinal fluid.
«So far our results are very preliminary – Angela Gritti comments. From what reported by the authors, the therapy was well tolerated but more time is needed to understand if it is effectively able to alter the natural history of this severe disease. A crucial issue that we hope to overcome with our approach, is to increase the amount of vector that actually reaches the brain cells and therefore to increase the amount of the functioning enzyme that can be produced. What makes things even more complex is also the fact that the enzyme is composed of two different subunits, which are encoded by two separate genes: this means that we need to deliver not just one but two genes, and with the correct ratios. This can be achieved by delivering either two different vectors together or one vector containing the genes for both subunits: the next experiments will help us understand which of these two possible strategies works best. It is good to see that for such complex and severe diseases there are more therapeutic approaches currently being studied. Moreover, the development of a strategy that allows to reach the brain effectively could also pave the way for the treatment of other diseases featuring the same ‘access issue’: for this reason, it is crucial to continue supporting research, as Fondazione Telethon does».